Low testosterone, commonly referred to as hypogonadism, is a condition characterized by diminished levels of the hormone testosterone. While the natural decline of testosterone is a normal part of aging, a substantial decrease can manifest a range of symptoms impacting various facets of physical, mental, and emotional well-being. This comprehensive exploration aims to delve deeper into the nuanced manifestations of low testosterone, offering in-depth insights into its profound effects and avenues for comprehensive care.
Must Read: Best Testosterone Boosters for Men Over 50 | Unlocking Vitality and Well-Being
Low Testosterone Symptoms
Contents
- 1 Low Testosterone Symptoms
- 2 Low Sex Drive (Libido):
- 3 Erectile Dysfunction:
- 4 Muscle Development:
- 5 Insomnia:
- 6 Fatigue:
- 7 Bone Loss:
- 8 Infertility:
- 9 Trouble Concentrating:
- 10 Depression:
- 11 Hair Loss:
- 12 Body Fat:
- 13 Enlarged Breasts (Gynecomastia):
- 14 Hot Flashes:
- 15 Irritability:
- 16 Shrinking Testicles:
- 17 Depressed Mood:
- 18 Gynaecomastia:
- 19 Loss of Body Hair:
- 20 Acne:
- 21 Decreased Energy:
- 22 Decreased Sexual Satisfaction:
- 23 Difficulty Concentrating:
- 24 Mood Swings:
- 25 Joint Pain:
- 26 Increased Cardiovascular Risk:
- 27 Increased Body Fatigue:
- 28 Memory Impairment:
- 29 Reduced Motivation:
- 30 Sleep Apnea:
- 31 Increased Risk of Type 2 Diabetes:
- 32 Decreased Libido in Women:
- 33 Thinning of Skin and Wrinkles:
- 34 Increased Sensitivity to Stress:
- 35 Reduced Physical Endurance:
- 36 Changes in Body Odor:
- 37 Causes of Low Testosterone
- 38 Testicle Injuries:
- 39 Cancer Treatments:
- 40 Stress:
- 41 AIDS:
- 42 Alcohol Use Disorder:
- 43 Kidney Disease:
- 44 Cirrhosis of the Liver:
- 45 Pituitary Gland Conditions:
- 46 Autoimmune Disease:
- 47 Infection:
- 48 Obesity:
- 49 Metabolic Syndrome:
- 50 Medications:
- 51 Optimizing Testosterone Levels
- 52 Natural Approaches:
- 53 Hormone Replacement Therapy (HRT):
- 54 Diet and Nutrition:
- 55 Exercise and Resistance Training:
- 56 Stress Management:
- 57 Avoiding Endocrine Disruptors:
- 58 Prescription Medications:
- 59 Regular Monitoring:
- 60 Potential Risks and Side Effects:
- 61 TestoGen: A Recommended Testosterone Booster:
- 62 Conclusion
- 63 Frequently Asked Questions (FAQs) on Low Testosterone Symptoms:
Low Sex Drive (Libido):
- Hormonal Influence: Testosterone plays a crucial role in regulating sexual desire by influencing brain receptors involved in sexual arousal. A decline in testosterone levels can lead to a diminished libido.
- Impact on Relationships: Beyond the physiological aspect, low libido can strain relationships due to the psychological implications. Open communication with a partner and healthcare professionals is crucial for addressing relationship dynamics.
Erectile Dysfunction:
- Quality of Erections: Testosterone contributes to the maintenance of penile tissue and blood flow, influencing the quality of erections. Low testosterone levels can lead to difficulties in achieving and sustaining satisfactory erections.
- Multidisciplinary Approach: Hormone replacement therapy, lifestyle modifications, and psychological interventions may be employed to address the multifaceted nature of erectile dysfunction.
Muscle Development:
- Beyond Mass: Testosterone is essential not only for muscle mass but also for muscle tone and definition. Low testosterone levels can contribute to a decrease in overall muscle quality.
- Comprehensive Approach: Integrating resistance training, a nutrient-rich diet, and potential hormone replacement therapy can collectively address the complexities of muscle development.
Insomnia:
- Bidirectional Relationship: Hormonal imbalances, including low testosterone, can disrupt sleep patterns, leading to insomnia. Adequate sleep hygiene, addressing underlying sleep disorders, and hormone replacement therapy may be considered for comprehensive management.
- Holistic Approach: Recognizing the interplay between hormonal balance and sleep, a holistic approach involves lifestyle modifications, cognitive behavioral therapy for insomnia (CBT-I), and potential hormonal interventions.
Fatigue:
- Beyond Tiredness: Low testosterone levels can contribute to a pervasive sense of fatigue, extending beyond physical tiredness to encompass mental and emotional exhaustion.
- Lifestyle Modifications: Strategies such as regular exercise, stress management, and adequate sleep are essential components of combatting fatigue associated with low testosterone.
Bone Loss:
- Increased Risk of Osteoporosis: Testosterone is crucial for maintaining bone density, and low levels can increase the risk of osteoporosis, especially in aging individuals.
- Comprehensive Management: In addition to regular bone density assessments, a comprehensive approach involves hormone replacement therapy, lifestyle modifications, and preventive measures such as adequate calcium and vitamin D intake.
Infertility:
- Sperm Production: Testosterone plays a vital role in the production of sperm. Low testosterone levels can affect sperm count and motility, contributing to fertility issues.
- Fertility Specialist Consultation: Collaborating with a fertility specialist can help develop a personalized treatment plan, which may include hormone replacement therapy and lifestyle modifications.
Trouble Concentrating:
- Cognitive Symptoms: Hormonal fluctuations, including low testosterone, can manifest as difficulties in concentration and memory lapses, impacting cognitive function.
- Comprehensive Approach: Addressing cognitive symptoms involves hormone replacement therapy, cognitive training exercises, and lifestyle modifications that support cognitive health.
Depression:
- Mood Disorders: Low testosterone has been linked to persistent feelings of sadness and a lack of interest, contributing to depressive symptoms.
- Collaborative Care: A collaborative approach involving endocrinologists and mental health professionals is crucial for managing depression associated with low testosterone.
Hair Loss:
- Complex Interaction: Testosterone’s conversion to dihydrotestosterone (DHT) is implicated in male pattern baldness. Understanding this interaction is crucial for exploring treatment options.
- Treatment Options: Alongside hormone replacement therapy, topical and oral medications, as well as hair transplant procedures, can be considered for managing hair loss.
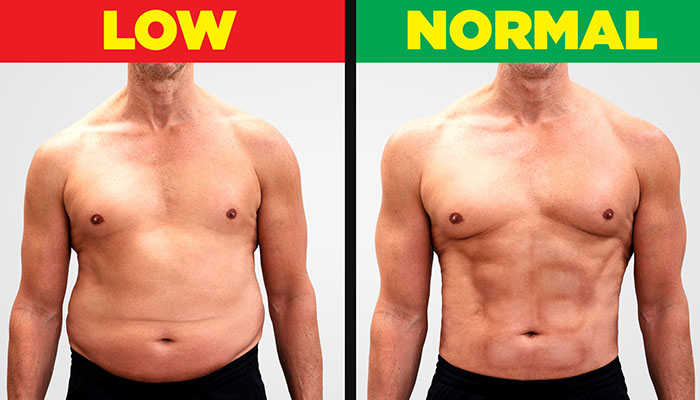
Body Fat:
- Changes in Fat Distribution: Testosterone influences fat metabolism, and low levels can contribute to changes in fat distribution, particularly an increase in visceral fat.
- Holistic Approach: Combining hormone replacement therapy with regular exercise and a balanced diet is essential for managing body fat and reducing associated health risks.
Enlarged Breasts (Gynecomastia):
- Hormonal Imbalance: The imbalance between testosterone and estrogen can result in the development of glandular tissue in male breasts.
- Treatment Options: Hormone replacement therapy, medications, or surgical interventions may be considered for addressing gynecomastia.
Hot Flashes:
- Menopausal Association: While commonly associated with menopause in women, men can also experience hot flashes with low testosterone levels.
- Management: Hormone replacement therapy and lifestyle modifications can help manage hot flashes in individuals with low testosterone.
Irritability:
- Behavioral Changes: Hormonal fluctuations, including low testosterone, can contribute to irritability and mood swings.
- Recognizing and Addressing: Strategies include hormone replacement therapy, stress management, and lifestyle modifications to address behavioral changes.
Shrinking Testicles:
- Visible Manifestation: Testicular atrophy, or shrinking of the testicles, can be a visible sign of hormonal imbalance.
- Thorough Evaluation: A healthcare professional’s assessment is necessary to determine the underlying cause and appropriate interventions.
Depressed Mood:
- Changes in Emotional States: Persistent sadness and lack of interest are emotional states linked to low testosterone.
- Collaborative Care: Involving endocrinologists and mental health professionals is crucial for addressing emotional changes associated with low testosterone.
Gynaecomastia:
- Beyond Physical Manifestation: Understanding the hormonal dynamics that contribute to the development of breast tissue in males.
- Thorough Evaluation: A healthcare professional’s assessment is necessary to determine the underlying cause and appropriate interventions.
Loss of Body Hair:
- Secondary Sexual Characteristics: Low testosterone levels can contribute to changes in body hair distribution, impacting one’s physical appearance.
- Aesthetic Consideration: Addressing concerns about changes in physical appearance may involve hormone replacement therapy and supportive aesthetic measures.
Acne:
- Hormonal Fluctuations: Testosterone’s influence on sebum production can contribute to acne development.
- Treatment Options: Exploring topical medications, oral antibiotics, and lifestyle modifications can help manage acne associated with low testosterone.
Decreased Energy:
- Pervasive Fatigue: Profound lack of motivation and reduced stamina can be indicative of low testosterone levels.
- Lifestyle Modifications: Strategies including regular exercise, a balanced diet, and stress management are essential for combating decreased energy.
Decreased Sexual Satisfaction:
- Impact Beyond Libido: Addressing challenges in achieving and maintaining erections is crucial for overall sexual satisfaction.
- Comprehensive Management: Involving hormonal interventions, psychological support, and communication with a partner is essential.
Difficulty Concentrating:
- Cognitive Symptoms: Manifestations such as difficulties in concentration and memory lapses require a comprehensive approach.
- Comprehensive Approach: Involving hormone replacement therapy, cognitive exercises, and lifestyle modifications is essential for addressing cognitive symptoms.
Mood Swings:
- Behavioral Changes: Mood swings can result from hormonal imbalances, impacting overall emotional well-being.
- Managing Fluctuations: Through hormone replacement therapy, stress management, and emotional support, individuals can better manage mood swings.
Joint Pain:
- Impact on Joint Health: Testosterone plays a role in maintaining joint health, and low levels can contribute to joint pain.
- Multifaceted Approach: Integrating hormone replacement therapy, joint-friendly exercises, and nutritional support is crucial for managing joint pain.
Increased Cardiovascular Risk:
- Correlation with Testosterone: Acknowledging the association between low testosterone and cardiovascular diseases is crucial.
- Proactive Measures: Emphasizing lifestyle modifications, regular exercise, and close monitoring of cardiovascular health can mitigate increased cardiovascular risk.
Increased Body Fatigue:
- Specific Aspect of Fatigue: Heightened tiredness even with minimal physical exertion may indicate low testosterone levels.
- Assessment and Intervention: Thorough evaluation of hormonal levels and potential hormone replacement therapy are key steps for addressing increased body fatigue.
Memory Impairment:
- Cognitive Impact: Linking low testosterone to difficulties in short-term and long-term memory recall requires a comprehensive approach.
- Holistic Approach: Combining hormone replacement therapy, cognitive exercises, and lifestyle modifications is essential for managing memory impairment.
Reduced Motivation:
- Psychological Aspect: Low testosterone levels can impact personal and professional goals, leading to reduced motivation.
- Intervention Strategies: Involving hormone replacement therapy and psychological support is crucial for rekindling motivation.
Sleep Apnea:
- Bidirectional Relationship: Recognizing the connection between low testosterone and sleep apnea is vital.
- Intervention: Lifestyle changes, positional therapy, and potential continuous positive airway pressure (CPAP) device usage can be considered for managing sleep apnea.
Increased Risk of Type 2 Diabetes:
- Link to Insulin Resistance: Understanding the association between low testosterone and insulin resistance is crucial for managing diabetes risk.
- Risk Management: Emphasizing lifestyle modifications, blood sugar monitoring, and collaboration with healthcare providers are essential for reducing the risk of type 2 diabetes.
Decreased Libido in Women:
- Testosterone’s Role in Females: Recognizing the impact on sexual desire in women is essential for comprehensive care.
- Comprehensive Management: Involving hormonal evaluations, lifestyle modifications, and potential hormone replacement therapy can address decreased libido in women.
Thinning of Skin and Wrinkles:
- Collagen Production: Testosterone plays a role in maintaining skin thickness and collagen production.
- Aesthetic Consideration: Addressing thinning skin and wrinkles may involve hormone replacement therapy and a tailored skincare regimen.
Increased Sensitivity to Stress:
- Impact of Hormonal Imbalances: Recognizing heightened sensitivity to stress is crucial for comprehensive care.
- Coping Strategies: Involving stress management techniques, mindfulness practices, and lifestyle modifications can help manage increased sensitivity to stress.
Reduced Physical Endurance:
- Testosterone’s Role in Performance: Understanding its impact on muscle development and endurance is essential.
- Gradual Improvement: Addressing reduced physical endurance through hormone replacement therapy and gradual increases in physical activity is crucial.
Changes in Body Odor:
- Hormonal Impact: Recognizing alterations in body odor due to hormonal imbalances is crucial.
- Management Strategies: Maintaining good personal hygiene, using deodorants, and addressing hormonal imbalances are essential components for managing changes in body odor.
Causes of Low Testosterone

Testosterone, a vital hormone for male reproductive health and overall well-being, naturally diminishes with age. However, beyond the natural aging process, various conditions and circumstances can contribute to low testosterone levels, presenting a complex interplay of factors that impact hormonal balance. Here, we delve into the multifaceted origins of low testosterone, shedding light on the diverse range of contributors:
Testicle Injuries:
- Traumatic incidents or injuries to the testicles can disrupt the delicate process of testosterone production, leading to a decline in overall levels.
Cancer Treatments:
- Aggressive cancer treatments, such as chemotherapy and radiation, designed to combat malignancies may inadvertently affect the testicles, impairing their ability to produce testosterone.
Stress:
- Chronic stress, a pervasive aspect of modern life, can elevate cortisol levels. The resulting hormonal imbalance may suppress the production of testosterone, affecting the delicate equilibrium.
AIDS:
- Individuals grappling with HIV/AIDS may experience disturbances in hormonal regulation, including a reduction in testosterone levels, further complicating the health challenges they face.
Alcohol Use Disorder:
- Excessive and prolonged alcohol consumption can disrupt the endocrine system, impacting the delicate dance of hormones and contributing to a decrease in testosterone production.
Kidney Disease:
- Impaired kidney function, whether due to disease or dysfunction, can disrupt the intricate hormonal balance, potentially leading to lower testosterone levels.
Cirrhosis of the Liver:
- Liver conditions, such as cirrhosis, can have cascading effects on hormonal metabolism, potentially interfering with testosterone production.
Pituitary Gland Conditions:
- Malfunctions in the pituitary gland, a master regulator of hormone production, can disturb the orchestration of hormones, including the signaling for testosterone synthesis.
Autoimmune Disease:
- Certain autoimmune conditions launch an assault on the body’s own cells, potentially including those responsible for testosterone production, leading to diminished hormone levels.
Infection:
- Infections affecting the testicles or glands involved in hormone regulation can disrupt the delicate balance, contributing to a decrease in testosterone.
Obesity:
- Excess body fat, particularly visceral fat, can induce a state of chronic inflammation and hormonal imbalance, culminating in lower testosterone levels.
Metabolic Syndrome:
- The cluster of conditions known as metabolic syndrome, encompassing obesity, high blood pressure, and insulin resistance, has associations with low testosterone, further complicating the hormonal landscape.
Medications:
- Certain medications, ranging from opioids to glucocorticoids and those used in prostate cancer treatment, can interfere with the endocrine system, potentially suppressing testosterone production.
Understanding these multifaceted contributors to low testosterone is crucial for developing targeted interventions and personalized treatment plans. It emphasizes the need for a comprehensive assessment by healthcare professionals to unravel the intricate web of factors influencing testosterone levels and address them effectively. As individuals navigate the complexities of hormonal health, tailored strategies can be employed to restore equilibrium and promote overall well-being.
Optimizing Testosterone Levels
Testosterone booster therapy encompasses a diverse range of strategies designed to address symptoms of low testosterone and enhance overall hormonal well-being. As we delve deeper into these approaches, it’s crucial to adopt a comprehensive, individualized plan that integrates both natural lifestyle adjustments and carefully selected therapeutic interventions. Let’s explore this in more detail:
Natural Approaches:
- The foundation of testosterone optimization lies in lifestyle modifications. Regular exercise, particularly resistance training and high-intensity interval training (HIIT), promotes not only muscle strength but also stimulates testosterone production. A well-balanced diet, rich in proteins, healthy fats, and essential nutrients like zinc and vitamin D, is integral to supporting overall hormonal health.
Hormone Replacement Therapy (HRT):
- HRT, involving the administration of exogenous testosterone, is a potent intervention for individuals with clinically low testosterone levels. Delivery methods include injections, gels, patches, or pellet implants. However, due to potential side effects, it requires careful monitoring and should only be pursued under the guidance of healthcare professionals.
Diet and Nutrition:
- A targeted nutritional approach plays a pivotal role in testosterone optimization. Specific nutrients, including zinc, vitamin D, and omega-3 fatty acids, contribute to hormone production. Supplements such as Testogen, enriched with testosterone-supportive ingredients like fenugreek extract and ginseng, can complement dietary efforts.
Exercise and Resistance Training:
- Tailored exercise regimens not only enhance physical fitness but also positively influence hormonal balance. Resistance training, in particular, stimulates testosterone production. Combining aerobic exercises with strength training provides a holistic approach to overall health and hormonal vitality.
Stress Management:
- Chronic stress, a common contributor to hormonal imbalances, necessitates effective management strategies. Incorporating mindfulness practices, relaxation techniques, and activities that promote emotional well-being can mitigate the negative impact of stress on testosterone levels.
Avoiding Endocrine Disruptors:
- Environmental factors, including exposure to endocrine-disrupting chemicals in plastics and pollutants, can interfere with hormonal balance. Adopting a lifestyle that minimizes exposure to these disruptors is a preventive measure for maintaining testosterone levels.
Prescription Medications:
- Healthcare professionals may prescribe medications to address specific hormonal imbalances. These medications, tailored to an individual’s health needs, require regular monitoring to ensure efficacy and mitigate potential side effects.
Regular Monitoring:
- Consistent monitoring of hormone levels is essential for assessing the effectiveness of chosen interventions. Regular check-ups with healthcare professionals allow for adjustments in the treatment plan based on individual responses and evolving health needs.
Potential Risks and Side Effects:
- While testosterone booster therapy can yield positive results, potential risks, and side effects should be thoroughly understood. Acne, fluid retention, and changes in red blood cell count are possible side effects. Long-term use without proper supervision may pose more serious health risks, underscoring the importance of professional guidance.
TestoGen: A Recommended Testosterone Booster:
- Testogen, a dietary supplement, stands out with its formulation of natural ingredients known to support testosterone production. Ingredients such as fenugreek extract, zinc, and vitamin D play crucial roles in hormonal balance. However, it’s crucial to recognize that individual responses to supplements can vary, emphasizing the need for consultation with healthcare professionals before incorporation.
Navigating the landscape of testosterone optimization demands a holistic, patient-centric approach. Collaborating with healthcare professionals ensures that interventions are tailored to individual needs, promoting not just hormonal health but overall well-being. By adopting a multifaceted strategy that combines natural lifestyle adjustments with carefully monitored therapeutic interventions, individuals can strive for hormonal vitality and an enhanced quality of life.
Conclusion
In conclusion, the exploration of low testosterone symptoms reveals a complex tapestry of interconnected manifestations affecting various aspects of health. Recognizing these symptoms and seeking comprehensive care are crucial steps for individuals to regain vitality, improve their quality of life, and foster overall well-being. Those experiencing these symptoms must prioritize consultation with healthcare professionals for thorough assessments and personalized interventions.
Through a combination of hormone replacement therapy, lifestyle modifications, and ongoing research advancements, individuals can navigate the complexities of low testosterone. A tailored and holistic approach ensures that each person’s unique set of symptoms and health considerations are addressed effectively.
Staying informed about emerging developments in the field of testosterone management allows both individuals and healthcare providers to make well-informed decisions. The integration of evolving research findings into treatment plans ensures that the management of low testosterone and its associated symptoms remains dynamic and effective.
In the journey towards optimal health, collaborative care involving endocrinologists, mental health professionals, fertility specialists, and other healthcare providers is essential. This collaborative approach ensures a comprehensive understanding of the multifaceted nature of low testosterone and facilitates the development of personalized interventions.
By fostering a proactive and informed approach, individuals can actively participate in their healthcare journey. Regular check-ups, open communication with healthcare providers, and adherence to prescribed interventions contribute to the ongoing management of low testosterone.
In essence, the exploration of low testosterone and its symptoms extends beyond a medical perspective; it involves a holistic understanding of how hormonal balance influences every facet of an individual’s well-being. With comprehensive care, individuals can navigate the complexities of low testosterone, fostering not just physical health but also emotional and mental resilience.
In conclusion, the journey through low testosterone is nuanced and multifaceted, demanding an individualized and comprehensive approach to care. As we delve deeper into the complexities of hormonal balance, we uncover a path toward optimal health, vitality, and an enhanced quality of life.
Frequently Asked Questions (FAQs) on Low Testosterone Symptoms:
- What are the common signs of low testosterone?
Common signs include low libido, erectile dysfunction, fatigue, muscle loss, and mood changes. However, symptoms can vary widely among individuals.
- Is low testosterone a normal part of aging?
Yes, testosterone levels naturally decline with age. However, pronounced decreases leading to noticeable symptoms may require attention and intervention.
- How does low testosterone affect sexual health?
Low testosterone can lead to a diminished sex drive, difficulty achieving and maintaining erections, and may contribute to infertility by affecting sperm production.
- Can low testosterone cause mental health issues?
Yes, low testosterone has been linked to mood disorders such as depression and irritability. It can also impact cognitive functions, including concentration and memory.
- Are there lifestyle factors that contribute to low testosterone?
Yes, factors such as obesity, lack of exercise, poor sleep, and chronic stress can contribute to low testosterone levels.
- What role does testosterone play in muscle development?
Testosterone is crucial for muscle development, including muscle tone and definition. Low levels can result in reduced muscle quality and increased body fat.
- Can low testosterone affect bone health?
Yes, low testosterone is associated with an increased risk of osteoporosis, highlighting its importance in maintaining bone density.
- Is there a connection between low testosterone and cardiovascular health?
Research suggests a correlation between low testosterone and cardiovascular diseases, emphasizing the need for proactive measures to manage cardiovascular health.
- Can low testosterone impact sleep quality?
Yes, hormonal imbalances, including low testosterone, can contribute to sleep disturbances and conditions like insomnia or sleep apnea.
- How is low testosterone diagnosed?
Diagnosis involves a blood test to measure testosterone levels, often in the morning when levels are highest. Other symptoms and medical history are also considered.
- What treatment options are available for low testosterone?
Treatment options include hormone replacement therapy, lifestyle modifications (such as exercise and a balanced diet), and addressing underlying health issues contributing to low testosterone.
- Is there a connection between low testosterone and diabetes?
Yes, low testosterone has been associated with insulin resistance, potentially increasing the risk of type 2 diabetes.
- Can women experience symptoms of low testosterone?
Yes, though women have lower testosterone levels than men, a decrease in testosterone can impact libido, mood, and overall well-being in women.
- Are there natural ways to boost testosterone levels?
Lifestyle changes such as regular exercise, a healthy diet, adequate sleep, and stress management can positively influence testosterone levels.
- How long does it take for testosterone therapy to show results?
Results vary, but many individuals may start to notice improvements in symptoms within a few weeks to months of starting testosterone therapy.
These FAQs provide general information, but it’s essential to consult with a healthcare professional for personalized advice and guidance based on individual health circumstances.


