Topical steroids
Contents
- 1 Topical steroids
- 2 What are topical steroids?
- 3 How do topical steroids work?
- 4 Types of topical steroids
- 5 Potency levels
- 6 Formulations
- 7 What conditions are treated with topical steroids?
- 8 How to use topical steroids
- 9 Precautions when using topical steroids
- 10 Side effects
- 11 Contraindications
- 12 Pre-existing medical conditions
- 13 How long should topical steroids be used?
- 14 Topical steroid withdrawal syndrome
- 15 Alternatives to topical steroids
- 16 FAQs
- 17 What is the strongest topical steroid?
- 18 Can topical steroids be used on the face?
- 19 Can topical steroids be used during pregnancy?
- 20 Can topical steroids be used on children?
- 21 How long does it take for topical steroids to work?
- 22 References:
Topical steroids are a type of medication that is frequently used to treat various skin conditions, including eczema, psoriasis, and dermatitis. These medications work by reducing inflammation and itching in the affected area, which can help to alleviate symptoms such as redness, swelling, and discomfort.
There are many different types of topical steroids available, and they vary in terms of their potency and strength. Some are very mild and are suitable for use on sensitive areas of the skin, while others are more potent and are used to treat severe or chronic skin conditions.
In this article, we will explore the different aspects of topical steroids, including how they work to reduce inflammation, the various types and potency levels available, and how to use them effectively. We will also discuss the potential side effects of topical steroids, as well as alternatives that may be used for those who are unable to tolerate these medications or prefer natural remedies. Whether you are someone who has been prescribed topical steroids or are simply interested in learning more about this type of medication, this article will provide you with the information you need to make informed decisions about your health and well-being.
Must Read: Top Oral Anabolic Steroids Of 2023 For Ultimate Results
What are topical steroids?
Topical steroids are a class of medications that are used to treat a variety of skin conditions. These medications contain corticosteroid hormones, which work by mimicking the effects of the body’s natural hormone cortisol. Cortisol plays an important role in regulating inflammation and immune responses in the body.
When applied topically to the skin, these medications are absorbed into the affected area, where they work to reduce inflammation, redness, itching, and other symptoms associated with skin conditions such as eczema, psoriasis, and dermatitis. Topical steroids are available in a variety of forms, including creams, ointments, gels, foams, and lotions, and can be prescribed in different strengths depending on the severity of the condition being treated.
Topical steroids are generally considered safe when used as directed by a healthcare professional. However, like all medications, they can have potential side effects, particularly if used over a long period of time or applied to large areas of the body. It is important to follow your healthcare provider’s instructions carefully and to report any unusual symptoms or side effects to your doctor right away. Additionally, if you are pregnant or breastfeeding, it is important to talk to your healthcare provider before using topical steroids to ensure that they are safe for you and your baby.
How do topical steroids work?
Topical steroids are a type of medication that is designed to reduce inflammation and itching in the skin. They work by suppressing the immune response and blocking the production of certain chemicals that cause inflammation, such as prostaglandins and leukotrienes. By reducing inflammation, topical steroids can help to alleviate symptoms associated with various skin conditions, such as redness, swelling, and pain.
In addition to reducing inflammation, topical steroids also work to reduce itching by suppressing the release of histamine, a chemical that causes itching. This can be particularly helpful for individuals with conditions such as eczema, psoriasis, or dermatitis, which can be accompanied by intense itching and discomfort.
Topical steroids are available in different strengths and formulations, depending on the severity of the skin condition being treated.
Types of topical steroids

Topical steroids are a type of medication that is commonly used to treat various skin conditions. They are classified according to their potency level, which determines how strong the medication is and how effective it is at reducing inflammation and itching. There are seven different classes of topical steroids, each with varying strengths and potencies.
Potency levels
Topical steroids are classified according to their potency level. There are seven different classes, ranging from the weakest (Class 7) to the strongest (Class 1). The potency level determines how strong the medication is and how effective it is at reducing inflammation and itching.
The potency levels of topical steroids are as follows:
Class 7 topical steroids are the weakest and are typically used to treat mild skin conditions, such as mild eczema or dermatitis. They are often recommended for use on the face or other sensitive areas of the skin, as they are less likely to cause side effects.
Class 6 topical steroids are slightly more potent than Class 7 and are used to treat mild to moderate skin conditions. They may be used on larger areas of the body but should still be used with caution.
Class 5 topical steroids are moderately potent and are used to treat moderate to severe skin conditions. They may be used on larger areas of the body but should be used with caution and for a limited period of time.
Class 4 topical steroids are potent and are typically used to treat severe skin conditions, such as psoriasis or severe eczema. They should only be used on small areas of the body for a limited period of time.
Class 3 topical steroids are very potent and are used to treat severe skin conditions that have not responded to other treatments. They should only be used on small areas of the body for a very limited period of time.
Class 2 topical steroids are extremely potent and are used to treat severe skin conditions that have not responded to other treatments. They should only be used under close medical supervision and for a very limited period of time.
Class 1 topical steroids are the strongest and are rarely used due to their potential for severe side effects. They should only be used under close medical supervision and for a very limited period of time.
It is important to note that the potency of a topical steroid does not necessarily correlate with its effectiveness. Your healthcare provider will determine the appropriate potency level based on the severity of your skin condition and other factors.
Formulations
Topical steroids are available in various formulations that are designed to be applied directly to the skin. The different formulations include creams, ointments, lotions, gels, and solutions. Each formulation has its own unique advantages and disadvantages, and the choice of formulation depends on the condition being treated and the skin type of the patient.
Creams are a popular formulation for topical steroids and are often recommended for conditions that are associated with weeping or oozing skin, as they are less greasy than ointments and can be absorbed more quickly. However, creams may not provide as much moisture as other formulations, which can be a concern for individuals with dry or sensitive skin.
Ointments are another common formulation for topical steroids and are often recommended for conditions that require a thicker, more emollient treatment. They are more occlusive than creams, meaning they create a barrier on the skin that helps to retain moisture. However, they can be greasy and may not be suitable for use on certain areas of the body, such as the face.
Lotions are a lighter formulation of topical steroids that are often recommended for use on larger areas of the body, such as the arms or legs. They are less greasy than creams and ointments and are often preferred by individuals with oily or acne-prone skin. However, they may not provide as much moisture as other formulations.
Gels are another option for topical steroids and are often recommended for use on areas of the skin that are difficult to treat with other formulations, such as the scalp or hairline. They are often clear and non-greasy and are absorbed quickly into the skin. However, gels may not provide as much moisture as other formulations.
Solutions are the most fluid formulation of topical steroids and are often used to treat conditions that affect the scalp or nails. They are easy to apply and can be used on hairy areas of the body. However, they may not provide as much moisture as other formulations and may be more difficult to apply to certain areas of the body.
Ultimately, the choice of formulation depends on the individual needs of the patient and the condition being treated.
What conditions are treated with topical steroids?
Topical steroids are an effective treatment for a variety of skin conditions, ranging from mild to severe. These medications are commonly prescribed to reduce inflammation and itching associated with conditions such as eczema, psoriasis, and dermatitis. In addition, they can be used to relieve symptoms associated with insect bites, rashes, hives, and poison ivy.
Eczema is a chronic condition characterized by dry, itchy, and inflamed skin. Topical steroids are often prescribed to reduce inflammation and relieve itching associated with eczema. Psoriasis is another chronic condition that causes red, scaly patches on the skin. Topical steroids can be used to reduce inflammation and help clear up psoriasis plaques.
Dermatitis is a term used to describe a variety of skin conditions that cause inflammation, including contact dermatitis and atopic dermatitis. Topical steroids are a common treatment for both types of dermatitis, as they help to reduce inflammation and itching.
Insect bites, rashes, and hives can also be treated with topical steroids. These conditions can cause redness, swelling, and itching, and topical steroids can provide quick relief of these symptoms.
Seborrheic dermatitis is a common skin condition that causes red, scaly patches on the scalp, face, and other areas of the body. Topical steroids can be used to reduce inflammation and relieve itching associated with seborrheic dermatitis.
Lichen planus is a condition that causes small, raised bumps on the skin, mouth, or genitals. Topical steroids can be used to reduce inflammation and relieve itching associated with this condition.
Finally, topical steroids can also be used to treat the symptoms of poison ivy, a plant that can cause an itchy, blistering rash upon contact. Topical steroids can help reduce the inflammation and itching associated with poison ivy rash, allowing for faster healing.
How to use topical steroids

When using topical steroids, it is important to follow the instructions provided by your healthcare provider. Typically, these medications are applied directly to the affected area once or twice a day, depending on the severity of the condition being treated and the potency of the medication.
Before applying the medication, it is important to wash and thoroughly dry the affected area. This helps to ensure that the medication is absorbed properly and reduces the risk of infection. It is also important to avoid using too much of the medication or applying it to areas of the skin that are not affected.
If you are using a cream or ointment, apply a thin layer to the affected area and gently rub it in. If you are using a lotion or gel, apply a small amount to the affected area and gently massage it in.
Precautions when using topical steroids
When using topical steroids, it is important to take certain precautions to ensure their safe and effective use. Some of these precautions include:
- Avoid using them on broken or infected skin, as this can increase the risk of absorption and systemic side effects.
- Do not use them for more than two to four weeks without medical supervision. Prolonged use can lead to skin thinning, stretch marks, and other potential side effects.
- Do not use them on the face unless directed by a healthcare provider. The skin on the face is thinner and more sensitive, which makes it more susceptible to side effects.
- Do not cover the affected area with airtight dressings, unless directed by a healthcare provider. This can increase the absorption of the medication and increase the risk of side effects.
- Use them sparingly to avoid side effects. Using too much of the medication or applying it to large areas of the body can increase the risk of side effects, including skin thinning, stretch marks, and increased susceptibility to infection.
Side effects
Topical steroids can cause side effects, especially when used for prolonged periods or in large amounts. The most common side effects of topical steroids include:
- Thinning of the skin (can make it more fragile and prone to tearing or bruising.)
- Stretch marks (can occur when the skin is stretched beyond its limits due to prolonged use of the medication.)
- Acne (can develop as a result of the increased oil production in the skin caused by the medication.)
- Rosacea (a skin condition that causes redness, bumps, and pimple-like lesions on the face.)
- Skin discoloration (can manifest as lightening or darkening of the skin.)
- Increased hair growth, (can occur in areas where the medication is applied.)
- Burning or stinging sensation, (especially when the medication is first applied.)
- Itching (can occur as a result of skin irritation caused by the medication.)
In rare cases, topical steroids can also cause more severe side effects, such as allergic reactions or skin infections.
Contraindications
Topical steroids are not recommended for use in people who have a hypersensitivity to the medication or any of its ingredients. They are also contraindicated in individuals with active tuberculosis, viral or fungal infections, or skin atrophy, as the medication can worsen these conditions.
In addition, topical steroids should not be used to treat acne rosacea or perioral dermatitis, as they can exacerbate these conditions. They are also contraindicated in people who have skin infections caused by bacteria, viruses, or fungi, as the medication can interfere with the body’s ability to fight off these infections.
Topical steroids should not be applied to open wounds, as they can delay the healing process and increase the risk of infection. If you have any of these conditions or are unsure whether topical steroids are appropriate for you, be sure to talk to your healthcare provider before using them.
Pre-existing medical conditions
People with pre-existing medical conditions, such as diabetes, should consult with their healthcare provider before using topical steroids. This is because some medical conditions can be aggravated by the use of topical steroids.
How long should topical steroids be used?
The duration of topical steroid treatment depends on the condition being treated and the severity of the symptoms. It is important to use topical steroids for the shortest amount of time possible to effectively manage symptoms and minimize the risk of side effects. Generally, topical steroids should not be used for more than two to four weeks without medical supervision.
If symptoms do not improve after two weeks of treatment or worsen during treatment, it is essential to consult a healthcare provider. In some cases, the provider may adjust the dose or change to a different medication. Additionally, if the condition being treated is chronic, long-term use of topical steroids may be necessary, but it should be closely monitored by a healthcare provider to minimize the risk of side effects.
Topical steroid withdrawal syndrome
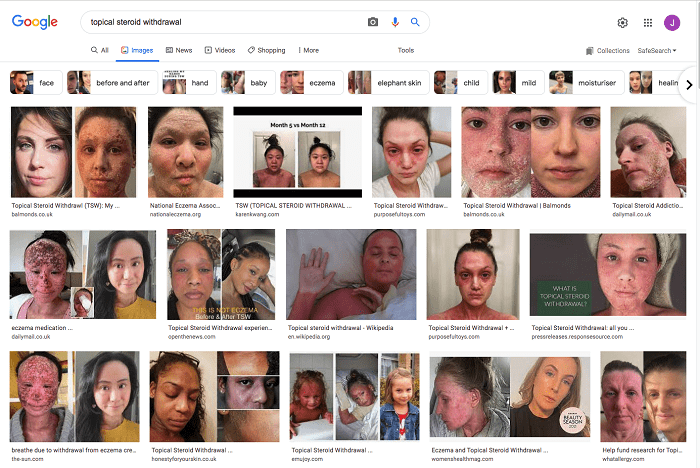
Topical steroid withdrawal syndrome (TSWS) is a rare but serious side effect of long-term use of topical steroids. TSWS can occur when an individual stops using topical steroids suddenly after prolonged use. This condition can be distressing and uncomfortable for those experiencing it, and can take several weeks or even months to resolve.
Some of the symptoms of TSWS include:
- Itching: This is a common symptom of TSWS and can be quite intense. The itching can be widespread or localized to the area where the topical steroid was applied.
- Burning or stinging sensation: Individuals experiencing TSWS may also feel a burning or stinging sensation in the affected area. This can be particularly uncomfortable if the skin is broken or has become sensitive due to the use of topical steroids.
- Redness: The affected area may also become red and inflamed. The redness can be widespread or localized to the area where the topical steroid was applied.
- Swelling: TSWS can also cause swelling in the affected area. The swelling can be mild or severe depending on the individual and the severity of their condition.
- Peeling skin: As the condition progresses, individuals may also experience peeling skin in the affected area. This can be particularly distressing if the skin is broken or sensitive.
If an individual is experiencing any of these symptoms after stopping the use of topical steroids, they should consult their healthcare provider for advice and treatment options. Treatment for TSWS may include the use of topical or oral medications to relieve symptoms and promote healing.
Alternatives to topical steroids
Topical steroids are a common treatment for skin conditions such as eczema, psoriasis, and dermatitis. However, there are other options available for individuals who may not want to use or have adverse reactions to topical steroids. Some of these alternatives include:
- Emollients: These are moisturizing agents that can help to soothe and hydrate the skin. Emollients come in many forms, including creams, lotions, and ointments. They work by forming a protective barrier over the skin to prevent water loss and reduce irritation. Emollients are often used alongside other treatments and can be used as a long-term maintenance strategy for skin conditions.
- Topical calcineurin inhibitors: These are medications that can help to reduce inflammation and itching in the skin without causing thinning of the skin. Examples of topical calcineurin inhibitors include pimecrolimus and tacrolimus. These medications are often used as an alternative to topical steroids for individuals with sensitive areas of skin, such as the face, neck, and genitals.
- Phototherapy: This is a treatment that uses ultraviolet light to reduce inflammation in the skin. Phototherapy can be done in a doctor’s office or at home using a special light box. It is often used to treat skin conditions such as psoriasis, eczema, and vitiligo. Phototherapy can be a safe and effective alternative to topical steroids for individuals who have not had success with other treatments.
It’s important to note that the best treatment option for a particular individual will depend on the severity of their skin condition, as well as their personal preferences and medical history. Individuals with skin conditions should work closely with their healthcare provider to find the most effective and appropriate treatment plan for their needs.
FAQs
What is the strongest topical steroid?
The strongest topical steroid is Class 1 (superpotent) steroids, such as clobetasol propionate.
Can topical steroids be used on the face?
Topical steroids can be used on the face, but only under the direction of a healthcare provider. This is because the skin on the face is thinner and more sensitive than other parts of the body, making it more prone to side effects.
Can topical steroids be used during pregnancy?
Topical steroids can be used during pregnancy, but only under the direction of a healthcare provider. This is because some topical steroids may be absorbed into the bloodstream and affect the developing fetus.
Can topical steroids be used on children?
Topical steroids can be used on children, but only under the direction of a healthcare provider. Children are more susceptible to side effects from topical steroids, such as thinning of the skin.
How long does it take for topical steroids to work?
The length of time it takes for topical steroids to work depends on the condition being treated and the potency of the medication. In some cases, the medication may start working within a few hours, while in others, it may take several days to a week for the medication to take effect.
References:
- American Academy of Dermatology (AAD) – https://www.aad.org/
- National Eczema Association (NEA) – https://nationaleczema.org/
- National Psoriasis Foundation (NPF) – https://www.psoriasis.org/
- Mayo Clinic – https://www.mayoclinic.org/
- MedlinePlus – https://medlineplus.gov/
- DermNet NZ – https://dermnetnz.org/
- British Association of Dermatologists (BAD) – https://www.bad.org.uk/
- American Society for Dermatologic Surgery (ASDS) – https://www.asds.net/
- National Institutes of Health (NIH) – https://www.nih.gov/
- Centers for Disease Control and Prevention (CDC) – https://www.cdc.gov/